[ez-toc]
Introduction of Insomnia and Depression
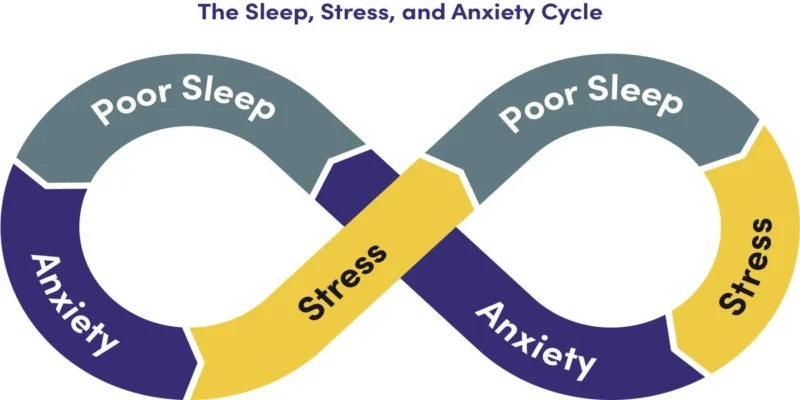
Insomnia and depression often go hand in hand, creating a complex relationship where one condition can both be a symptom of and a risk factor for the other.
There’s a two-way link between insomnia and depression. Sleep problems can be both a symptom of and a risk factor for depression.
Insomnia can mean having trouble falling asleep, staying asleep, or waking up at a desired time. Basically, you aren’t getting enough sleep to function well. Depression can range from having a few depressive symptoms to major depression.
In this guide, we’ll examine how these two conditions can come together. We’ll also look at treatment options if you have insomnia and depression.
The Interconnection between Depression and Insomnia

Depression, characterized by a range of depressive symptoms, can be exacerbated by poor sleep quality. Research has shown a significant association between insomnia and an increased risk of depression.
Several theories attempt to explain this link:
- Cognitive and Mood Changes: Sleep deprivation can lead to cognitive impairment and mood fluctuations, potentially contributing to the development or exacerbation of depression.
- Emotional Regulation and Neural Processes: Sleep disturbances may disrupt emotional regulation and stability, as well as alter neural processes within the brain.
- Stress Response and Inflammatory Markers: Lack of sleep can induce a stress response in the body and elevate levels of inflammatory markers, which may further contribute to the development of depression.
A two-way street exists between insomnia and depression, as evidence suggests that having one condition increases the risk of developing the other.
In fact, insomnia is a more consistent predictor of depression compared to the reverse relationship.
High Ratio of Sleep Complaints in Depression

Research indicates that approximately 90 percent of individuals with depression report experiencing sleep-related complaints.
These complaints may include insomnia, narcolepsy, disordered breathing, or restless legs syndrome (RLS). Dr. David A. Merrill, a psychiatrist specializing in adult and geriatric care, confirms this observation based on his clinical experience, noting that disrupted sleep is a core feature of depression.
In some cases, insomnia can manifest as part of a severe major depressive episode, requiring dedicated treatment.
Prioritizing Treatment: Addressing Insomnia or Depression First?
The approach to treating insomnia and depression depends on the individual’s circumstances.
Typically, healthcare providers prioritize addressing the condition that the patient identifies as the primary problem.
For example, if depression is the primary concern, the doctor may prescribe an antidepressant to improve mood, which could subsequently lead to better sleep.
Also Read: Tai Chi for Weight Loss: Enhancing Your Fitness
On the other hand, if sleep disturbances are the primary complaint, a sleeping aid might be recommended.
However, it is crucial to note that long-term use of sleeping pills lacks robust evidence and may not effectively treat chronic insomnia.
In some cases, effectively treating depression can alleviate sleep problems.
The complex relationship between these two conditions emphasizes the importance of individualized treatment plans tailored to each person’s specific needs.
Non-Medication and Natural Treatment Options

Various non-medication and natural treatment options can help improve sleep quality and address symptoms of depression.
These strategies include:
- Cognitive Behavioral Therapy (CBT): CBT is the first-line treatment for insomnia and is often used to manage depression as well. This short-term therapy, facilitated by a mental health professional, helps individuals identify and modify thoughts and behaviors associated with both insomnia and depression. Additional techniques, such as sleep hygiene and relaxation exercises, may complement CBT for better sleep quality.
- Relaxation Techniques: Practices like deep breathing, visualization, progressive muscle relaxation, and biofeedback are frequently recommended for addressing insomnia. A recent meta-analysis confirms the safety and potential effectiveness of relaxation techniques in reducing depression symptoms when practiced regularly.
- Exercise: Engaging in regular physical exercise has been shown to improve self-reported sleep quality, insomnia severity, and daytime sleepiness. Additionally, exercise, especially when combined with medication, has demonstrated efficacy in treating depression, as evidenced by a review of 22 studies.
- Mind-Body Practices: Research suggests that mind-body practices, such as yoga, tai chi, qigong, and meditation, can improve symptoms of insomnia and overall well-being. Although studies on the impact of yoga on depression have been limited in size and duration, a 2017 review suggests its potential benefits.
Certain natural supplements may also positively impact mood and sleep. However, it is essential to consult with a physician, particularly when combining supplements with existing medications.
Some supplements believed to have potential benefits include valerian root, magnesium, passionflower, lavender, and tryptophan.
Medications for Insomnia and Depression

Medication for insomnia
If you have depression, check with your doctor before trying over-the-counter (OTC) sleep aids.
Prescription sleep medications fall under several categories, including:
- benzodiazepine receptor agonists: triazolam, temazepam, estazolam, lorazepam
- non-benzodiazepine receptor agonists: eszopiclone (Lunesta), zaleplon (Sonata), zolpidem (Ambien)
- melatonin receptor agonists: ramelteon (Rozerem)
- histamine receptor agonists: doxepin (Silenor)
- orexin receptor agonists: suvorexant (Belsomra), lemborexant (Dayvigo)
Medications approved for depression
There are many types of drugs used to treat depression.
Among them are:
- selective serotonin reuptake inhibitors (SSRIs)
- serotonin and norepinephrine reuptake inhibitors (SNRI)
- atypical antidepressants
- tricyclic and tetracyclic antidepressants
- monoamine oxidase inhibitors (MAOIs)
When insomnia and depression coexist, it is crucial to consider the use of medications for both conditions.
Antidepressants are commonly prescribed for depression, but their potential effects on sleep quality must be considered.
Some antidepressants may have sedating properties, making them useful for treating insomnia associated with depression.
However, certain older antidepressants may cause memory impairment or other adverse effects, necessitating caution.
Prescription sleep medications fall into different categories, such as benzodiazepine receptor agonists, non-benzodiazepine receptor agonists, melatonin receptor agonists, histamine receptor agonists, and orexin receptor agonists.
These medications are typically intended for short-term use, as long-term reliance on sleeping pills can lead to dependence and decreased efficacy.
Combining multiple sedative medications can also result in adverse side effects, such as daytime fatigue, confusion, and slowed reaction time.
It is advisable to focus on addressing the root causes of sleep disturbances by treating depression during the day, thereby improving sleep quality naturally.
Various types of drugs, such as selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors (SNRIs), atypical antidepressants, tricyclic and tetracyclic antidepressants, and monoamine oxidase inhibitors (MAOIs), are prescribed to treat depression.
Some antidepressants have sedating effects, making them suitable for managing insomnia independently of depression.
Notably, all antidepressants can improve sleep secondary to mood in the long term, but certain types may impair sleep in the short term.
Collaboration with a healthcare provider is vital to identify the most appropriate medication and monitor for any new or worsening symptoms.
Seeking Professional Help
Individuals experiencing chronic insomnia, defined as trouble falling or staying asleep at least three times a week for over three weeks, should seek evaluation by a physician.
Recognizing the severity of depression and its potential impact on sleep, it is crucial to consult with a mental health professional for an accurate diagnosis and tailored treatment plan.
Professional guidance is essential to determine the most suitable treatment options and address the unique needs of each individual.
Summary
Even the most severe cases of depression can be effectively treated, and initiating treatment early tends to yield better results.
Antidepressants may take several weeks to demonstrate their full effect, and improvements in sleep problems often precede improvements in mood.
While insomnia can be successfully treated through a combination of sleep hygiene adjustments and cognitive behavioral therapy, it is essential to note that for some individuals, particularly those with severe insomnia, the condition may persist.
Attempting to manage insomnia and depression without professional assistance can be hazardous.
Every individual is unique, and a healthcare provider can help identify specific needs and determine the most suitable treatment options.
With the right support and comprehensive treatment approach, individuals can reclaim their sleep quality and regain control over their mental well-being.






Your mode of telling everything in this post is really fastidious, every one
can without difficulty understand it, Thanks a lot.
Thanks designed for sharing such a pleasant thinking, article
is good, thats why i have read it fully