Tardive dyskinesia (TD) is a serious movement disorder that often occurs as a side effect of long-term use of certain medications, particularly antipsychotics.
This condition involves involuntary, repetitive body movements that can affect various parts of the body, including the face, limbs, and torso. Understanding TD is crucial for patients and healthcare providers to manage and treat this challenging disorder effectively.
What is Tardive Dyskinesia?
Tardive dyskinesia is a neurological disorder characterized by involuntary, repetitive movements that can range from mild to severe. These movements are often slow, writhing, and can be disfiguring or disabling.
TD typically results from prolonged use of antipsychotic drugs, which are commonly prescribed for mental health conditions such as schizophrenia, bipolar disorder, and severe depression.
Symptoms of Tardive Dyskinesia
Recognizing the symptoms of tardive dyskinesia (TD) is crucial for timely intervention and management.
The disorder manifests through a variety of involuntary, repetitive movements that can affect different parts of the body.
Here are the primary symptoms to watch for:
- Facial Movements:
- Grimacing
- Lip smacking
- Puckering and pursing of the lips
- Rapid eye blinking
- Tongue movements, including sticking out the tongue or tongue thrusting
- Limb Movements:
- Jerking or twitching of the arms, legs, fingers, and toes
- Complex movements such as writhing or squirming
- Involuntary tapping or drumming of the fingers
- Torso Movements:
- Swaying or twisting of the torso
- Hip thrusting or rocking movements
These movements can vary in severity and frequency. They often become more pronounced over time, particularly if the use of the causative medication continues.
Identifying these symptoms early is essential for minimizing the long-term impact of the disorder and improving the patient’s quality of life.
Causes and Risk Factors
Tardive dyskinesia (TD) primarily results from prolonged use of certain medications, especially antipsychotics.
Understanding the causes and identifying the risk factors can help in preventing and managing this condition effectively.
Causes of Tardive Dyskinesia
The main cause of TD is long-term use of antipsychotic drugs, which are commonly prescribed to treat mental health conditions such as schizophrenia, bipolar disorder, and severe depression.
These medications work by blocking dopamine receptors in the brain to control psychiatric symptoms.
However, prolonged interference with dopamine, a neurotransmitter essential for regulating movement, can lead to the development of TD.
Also Read: Comprehensive Guide to Understanding Chlamydia
Other medications that may cause TD include:
- Antiemetics: Drugs used to control nausea and vomiting, such as metoclopramide (Reglan).
- Antidepressants: Certain types can also contribute to the development of TD.
- Mood Stabilizers: Used in treating mood disorders, these can sometimes have similar side effects.
Risk Factors for Tardive Dyskinesia
Several factors increase the likelihood of developing tardive dyskinesia, including:
- Duration of Antipsychotic Use: The risk of developing TD increases with the length of time these medications are used. Long-term use significantly raises the likelihood of experiencing symptoms.
- Type of Antipsychotic Medication: First-generation (typical) antipsychotics, such as haloperidol (Haldol) and chlorpromazine (Thorazine), have a higher association with TD compared to second-generation (atypical) antipsychotics like clozapine (Clozaril) and quetiapine (Seroquel).
- Age: Older adults are at a higher risk of developing TD, likely due to age-related changes in drug metabolism and sensitivity.
- Gender: Women are more prone to developing TD, possibly due to hormonal differences that affect drug metabolism.
- Underlying Medical Conditions: Individuals with pre-existing mental health disorders, diabetes, or a history of substance abuse are more susceptible to developing TD.
- Genetic Factors: Some individuals may have a genetic predisposition that makes them more vulnerable to TD.
Other Contributing Factors
- Dosage: Higher doses of antipsychotic medications can increase the risk of developing TD.
- Treatment Interruption: Sudden discontinuation or frequent changes in medication can trigger or worsen symptoms.
- Individual Sensitivity: Some people may be more sensitive to the effects of antipsychotic drugs, even at lower doses.
Understanding these causes and risk factors is vital for both healthcare providers and patients.
It helps in making informed decisions about medication use and in implementing strategies to minimize the risk of developing tardive dyskinesia.
Regular monitoring and early intervention can significantly improve outcomes for those at risk.
Diagnosing Tardive Dyskinesia
Diagnosing tardive dyskinesia (TD) involves a comprehensive evaluation by healthcare professionals to ensure accurate identification and management of the disorder.
The diagnostic process includes several steps:
Clinical Evaluation
The first step in diagnosing TD is a detailed clinical evaluation.
This involves:
- Medical History Review: The healthcare provider will review the patient’s complete medical history, including the duration and type of medications used, particularly antipsychotics and other drugs associated with TD.
- Symptom Assessment: A thorough assessment of the patient’s symptoms, focusing on the type, frequency, and severity of involuntary movements. The provider will observe the patient for specific signs of TD, such as facial grimacing, lip smacking, and limb movements.
Physical Examination
A physical examination is conducted to rule out other conditions that might cause similar symptoms.
This includes:
- Neurological Examination: To evaluate the functioning of the nervous system and identify any abnormalities in movement or coordination.
- Motor Function Tests: Tests to assess the patient’s muscle strength, reflexes, and range of motion.
Use of Diagnostic Scales
To quantify the severity of TD and track changes over time, healthcare providers often use standardized diagnostic scales, such as:
- Abnormal Involuntary Movement Scale (AIMS): This scale measures the presence and severity of involuntary movements in various parts of the body. It involves a series of questions and observations that help in grading the extent of TD symptoms.
- Extrapyramidal Symptom Rating Scale (ESRS): This tool assesses both the severity of TD and other drug-induced movement disorders.
Differential Diagnosis
It’s crucial to differentiate TD from other movement disorders that have similar presentations.
This process might involve:
- Blood Tests: To check for metabolic abnormalities or other underlying conditions.
- Imaging Studies: MRI or CT scans may be used to rule out other neurological disorders.
- Electromyography (EMG): This test measures the electrical activity of muscles to detect any abnormal muscle contractions.
Patient and Family Interviews
Interviews with the patient and their family members can provide additional insights into the onset and progression of symptoms, as well as the impact on daily life. This information is valuable for understanding the context of the symptoms and any potential triggers.
Medication Review and Adjustment
Sometimes, the diagnosis is confirmed by observing changes in symptoms after adjusting the patient’s medication regimen.
This might include:
- Reducing Dosage: Gradually lowering the dose of the causative antipsychotic to see if symptoms improve.
- Switching Medications: Changing to a different medication with a lower risk of causing TD can help determine if the previous medication was responsible for the symptoms.
Treatment Options for Tardive Dyskinesia
Managing tardive dyskinesia (TD) involves a combination of strategies aimed at reducing symptoms and improving the patient’s quality of life. While there is no definitive cure for TD, various treatment options can help manage the condition effectively.
Medication Adjustments
One of the first steps in treating TD is reviewing and adjusting the medications that may be causing the symptoms:
- Reducing or Discontinuing Antipsychotics: If feasible, gradually reducing the dose of the antipsychotic medication may help alleviate symptoms. However, this must be done under close medical supervision to avoid exacerbating the underlying psychiatric condition.
- Switching to Atypical Antipsychotics: Transitioning to second-generation (atypical) antipsychotics, which have a lower risk of causing TD, can be beneficial. Medications like clozapine (Clozaril) and quetiapine (Seroquel) are often considered.
Medications Specifically for Tardive Dyskinesia
Several medications are approved for the treatment of TD. These drugs help manage the involuntary movements by modulating neurotransmitter activity in the brain:
- Deutetrabenazine (Austedo): This medication reduces dopamine levels, helping to control the abnormal movements associated with TD.
- Valbenazine (Ingrezza): Similar to deutetrabenazine, valbenazine works by inhibiting the transport of dopamine, thus reducing involuntary movements.
Botulinum Toxin Injections
For focal dystonia or specific muscle groups affected by TD, botulinum toxin (Botox) injections can be effective. These injections temporarily paralyze the overactive muscles, reducing the severity of involuntary movements.
Non-Pharmacological Treatments
In addition to medication, several non-pharmacological treatments can support the management of TD:
- Physical Therapy: Regular physical therapy sessions can help improve muscle control, coordination, and overall physical function.
- Speech Therapy: For individuals experiencing orofacial dyskinesia, speech therapy can aid in improving communication and swallowing difficulties.
- Occupational Therapy: Occupational therapy can assist in developing strategies to perform daily activities more effectively, despite movement challenges.
Lifestyle and Supportive Measures
Implementing lifestyle changes and supportive measures can significantly impact the management of TD symptoms:
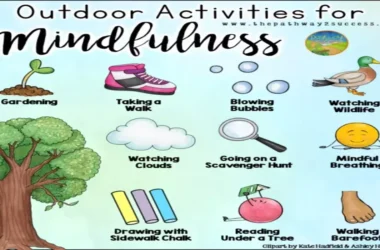
- Stress Management: Techniques such as mindfulness, meditation, and relaxation exercises can help reduce stress, which may exacerbate TD symptoms.
- Balanced Diet and Hydration: Maintaining a healthy diet and staying well-hydrated can support overall health and potentially alleviate some symptoms.
- Regular Exercise: Engaging in regular physical activity can improve overall well-being and help manage the physical manifestations of TD.
Support and Counseling
Living with TD can be challenging both physically and emotionally. Support groups and counseling can provide valuable emotional support and practical advice:
- Support Groups: Connecting with others who have TD can provide a sense of community and shared understanding, helping individuals cope with their condition.
- Professional Counseling: Mental health professionals can offer strategies to manage the emotional and psychological impact of living with TD.
Ongoing Monitoring and Research
Continuous monitoring of TD symptoms and treatment efficacy is essential. Healthcare providers should regularly evaluate the patient’s condition and adjust the treatment plan as necessary. Additionally, staying informed about ongoing research and emerging treatments can offer new avenues for managing TD.
Lifestyle and Supportive Measures
In addition to medical treatments, several lifestyle changes and supportive measures can help manage tardive dyskinesia symptoms:
- Physical Therapy: Regular physical therapy can improve muscle control and reduce the severity of involuntary movements.
- Speech Therapy: For individuals experiencing facial and oral movements, speech therapy can aid in improving communication and swallowing difficulties.
- Stress Management: Techniques such as mindfulness, meditation, and relaxation exercises can help reduce stress, which may exacerbate TD symptoms.
- Nutritional Support: A balanced diet and adequate hydration can support overall health and well-being, potentially mitigating some symptoms.
Living with Tardive Dyskinesia
Living with tardive dyskinesia can be challenging, but with the right support and management strategies, individuals can maintain a good quality of life.
It’s important to work closely with healthcare providers to tailor a treatment plan that addresses both the physical and psychological aspects of the disorder. Support groups and counseling can also provide emotional support and practical advice for managing daily challenges.
Future Directions and Research
Research on tardive dyskinesia is ongoing, with efforts focused on better understanding the underlying mechanisms, improving diagnostic methods, and developing more effective treatments. Advancements in pharmacology and neurology hold promise for future breakthroughs that could offer more hope for those affected by TD.
Conclusion
Tardive dyskinesia is a complex and often debilitating disorder resulting from long-term use of antipsychotic medications. Understanding its symptoms, causes, and treatment options is crucial for effective management.
Through medical interventions, lifestyle adjustments, and ongoing support, individuals with TD can achieve a better quality of life. Staying informed about the latest research and treatment developments can also provide additional pathways to managing this challenging condition.